Multiple Pregnancy Scans
From 7+ weeks
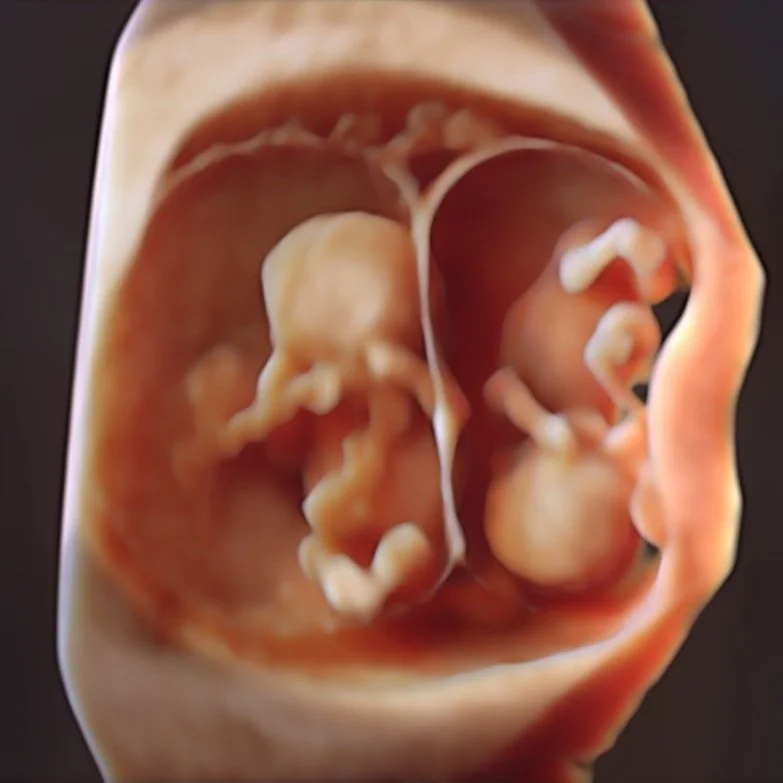
Multiple pregnancy Scans
When a woman is pregnant with twins, triplets, quads, or more, a multiple pregnancy scan, also known as a multiple gestation ultrasound, is conducted to provide a comprehensive examination. Multiple pregnancies account for approximately 1.8% of all pregnancies and are more likely to occur as the mother's age increases or with the use of assisted reproductive technologies such as in vitro fertilization (IVF) and ovulation induction. While most multiple pregnancies have positive outcomes, there is a higher risk of complications for both the mother and babies, with premature delivery being the most common complication. A multiple pregnancy scan involves thorough monitoring to address the heightened potential for complications. During a multiple pregnancy scan, several important components are typically included to ensure the health and well-being of both the mother and the babies:
Determining the number of fetus’ and the type of placenta: An early ultrasound is used to confirm the number of fetus’ and whether they share a placenta, which is crucial for assessing potential risks.
Monitoring growth: Regular scans are performed to track the growth of each baby and compare it to standard growth charts to detect any signs of growth restriction.
Checking for Twin-to-Twin Transfusion Syndrome (TTTS): If the babies share a placenta, they are at risk of developing TTTS, a condition where blood from one twin is transferred to the other. This is carefully assessed during the scan.
Assessing amniotic fluid: The amount of amniotic fluid around each baby is measured to identify any imbalances, which can be indicative of complications such as TTTS.
Checking fetal anatomy: Each baby's anatomy is evaluated in detail to check for any developmental abnormalities.
Assessing the cervix: The length and appearance of the cervix are assessed to identify any signs of preterm labour, which is more common in multiple pregnancies.
These scans are essential for monitoring the progress of the pregnancy and ensuring the best possible outcomes for both the mother and the fetus’.
Understanding Different Types of Multiple Pregnancies
Dichorionic
This is the most common type of spontaneous twin pregnancy, where the mother releases two eggs, both of which are fertilized. These twins, also known as non-identical or fraternal twins, each form their own placenta, resulting in a dichorionic twin pregnancy. In this type of pregnancy, if something affects one twin, it does not directly impact the other, as they have separate circulations.
Monochorionic
In this type of twin pregnancy, a single egg is fertilized, and the early embryo splits into two, resulting in identical twins. Most often, this splitting occurs a few days after conception, leading to the formation of a single placenta for both babies, known as a monochorionic placenta. In these cases, the twins share a single placenta, and there are blood vessel connections on the surface of the placenta that link the circulations of the two twins. While these connections typically balance the blood flow between the twins, in some cases, imbalances can lead to major complications such as Twin-twin transfusion syndrome (TTTS), acute transfusion TAPS, and TRAP.
Understanding the type of multiple pregnancy is crucial for providing appropriate prenatal care and monitoring to ensure the health and well-being of both the mother and the fetus’.
Diamniotic & Monoamniotic Twins
In most cases, twins are enclosed in their own amniotic sacs, a condition referred to as diamniotic. However, if the embryo splits late in development, the twins may share the same amniotic sac, known as monoamniotic. In rare instances, if the split occurs very late, the twins may only partially separate, resulting in conjoined twins.
It's important to note that identical twins, despite sharing the same genetic makeup, may split very early in development and each form their own placenta. As a result, some identical twins may have dichorionic placentas, adding a layer of complexity to the understanding of twin pregnancies.
Understanding the specific characteristics of each type of twin pregnancy is essential for providing the appropriate medical care and support for expectant mothers and their fetus’.
Twin-Twin Transfusion Syndrome
Twin-Twin Transfusion Syndrome (TTTS) is a significant complication that can arise in monochorionic pregnancies, where twins share the same placenta. Typically, multiple blood vessels connect the circulations of the twins on the surface of the shared placenta, allowing for balanced blood circulation between them. While most monochorionic twins have their own amniotic sac, approximately 10% of these pregnancies experience unbalanced connections between the twins, leading to a chronic transfusion of blood from one twin (the donor) to the other twin (the recipient). This condition usually develops in mid-pregnancy, between 16 and 28 weeks.
As a result of this unequal blood flow, both twins respond differently. The donor twin attempts to compensate for the blood volume loss by reducing its urine output. Since most of the amniotic fluid around the baby is composed of urine produced by the baby, this compensation leads to a significant decrease in the amount of fluid around the donor twin. In more severe cases, the amnion is observed to wrap around the donor twin, and in the most serious cases, no fluid is seen around the donor twin, causing it to appear "stuck."
It is crucial to carefully monitor monochorionic pregnancies for signs of TTTS and to provide appropriate interventions to ensure the best possible outcomes for both twins and the mother.
The twin that receives the blood transfusion is referred to as the recipient twin. In response to the increased blood volume, the recipient twin significantly increases its urine output, leading to the excessive accumulation of amniotic fluid, a condition known as polyhydramnios. This rapid increase in the mother's abdominal size over a few weeks may be noticeable. If left untreated, polyhydramnios can lead to the expansion of the mother's uterus well beyond the size expected for a full-term pregnancy. This can result in preterm labour, premature rupture of the membranes, or the loss of one or both twins in utero. If left untreated, very few, if any, of these twins would survive, as TTTS typically develops in mid-pregnancy.
Additionally, the transfusion process can have other effects on the recipient twin. The twin's heart may enlarge in an attempt to cope with the extra blood volume, and ultimately, its ability to pump may fail, leading to heart failure and fetal hydrops.
As a result of the TTTS process and the consequences of the transfusion for both twins, it is possible that one or both of the twins may be lost without warning. In the event that one twin survives, it may face long-term major injury as a result of the TTTS process.
Upon diagnosis, TTTS can be staged to determine its severity, which in turn guides treatment options. In some cases, twins may present with very early Stage 1 TTTS, and observation may be recommended as it has the potential to resolve spontaneously. However, if there is any progression or if the TTTS advances to more severe stages (Stage 2 to 4), fetal surgery with laser ablation is a common treatment option with a favourable success rate.
Staging TTTS for severity and considering appropriate treatment options is essential for addressing the condition and improving the chances of a positive outcome for both twins and the expectant mother.
-
To acquire the best diagnostic images possible, the examination is routinely performed Transabdominally, sometimes followed by a Transvaginal ultrasound (always with your written consent first).
-
In most cases the examination will be performed transabdominally, but there are some situations where a Transvaginal ultrasound maybe necessary. This improves the assessment of the cervix, placenta and obtain better details of the fetus. In turn this can improve accuracy if the diagnosis.
Transabdominal and transvaginal ultrasound examinations are safe at all stages of pregnancy.
-
The ultrasound procedure typically lasts anywhere from 30-90 minutes. However, the duration may vary depending on the specific reason for the examination and the complexity of the individual case.
-
If possible we recommend wearing comfortable, loose-fitting clothing that provides easy access to the area being imaged. Two-piece clothing, with separate upper and lower garments, is preferable.
Additionally, please ensure that you empty your bladder 1 hour before the procedure and then drink 2 glasses (600ml) of water, holding it without emptying your bladder again. Please note that your appointment might be delayed if your bladder is not adequately full.
-
Having some urine in your bladder can be beneficial for outlining the cervix and visualizing the relationship of the placenta with the lower uterus during imaging. It also helps to elevate the uterus from the pelvis into the abdomen, facilitating better visualization of the fetus.
You don't need to have a large amount of urine, and simply drinking a glass of water 30-60 minutes before your scheduled appointment is sufficient.
-
We welcome one adult support person, whether it be your partner or a family member, to accompany you during your Diagnostic scan. However, for specific reasons, we have implemented policies that prohibit children from attending Diagnostic ultrasound appointments. While we understand that this may be disappointing for families, it is essential to maintain a focused environment. Thus allowing the Sonographer to be able to concentrate during the scan whilst taking the necessary images and measurements. Occasionally, our sonographer may need to discuss unfortunate news found during your appointment and so this must be taken into consideration. The presence of children can introduce distractions that may impact the quality of the examination.
-
At Trinity Imaging, we provide our patients with their images to an app on your phone called Tricify. For further details please ask our receptionist at your appointment.

Our Dating Scans take up to 30 minutes and include:
2 x 3D thermal printed hard copy images
All pictures taken on the day straight to your mobile phone
Our Nuchal Scans take up to 90 minutes and include:
2 x 3D thermal printed hard copy images
All pictures taken on the day straight to your mobile phone
Our Early Anatomy Scans take up to 90 minutes and include:
2 x 3D thermal printed hard copy images
All pictures taken on the day straight to your mobile phone
Our Growth Scans take up to 60 minutes and include:
2 x 3D thermal printed hard copy images
All pictures taken on the day straight to your mobile phone
All our scans are performed in our premium-furnished luxury viewing room specially designed for you.
We are all looking forward to getting to know you, your baby and family along your pregnancy journey.