Preeclampsia Screening
From 13+ weeks
Preeclampsia Screening
Preeclampsia is a serious complication of pregnancy that can affect the mother and fetus/ fetus’. It is the most common medical condition in pregnancy that can cause high blood pressure, swelling, along with rapid weight gain due to the fluid retention and protein in the urine. It can range from mild to severe and can affect various systems of the body. Preeclampsia frequently coexists with poor placental function (placental insufficiency). It can therefore restricts the baby’s growth and also causes premature separation of the placenta (placental abruption).
Preeclampsia is the leading cause of medically indicated preterm birth when it is diagnosed in pregnancy.
Preeclampsia affects 2-5% of pregnant women of whom about 1 in 200 can suffer from severe Preeclampsia arising before 34 weeks of pregnancy. Early screening for Preeclampsia is important as early intervention (before 16 weeks) can reduce the effects for both mum and fetus.
Preeclampsia screening involves:
Measurement of maternal mean arterial blood pressure.
A blood test at 10 weeks to assess pregnancy associated plasma protein A (PAPP-A) and placenta growth factor (PIGF)
Assessing maternal height and weight.
Assessing Maternal medical history
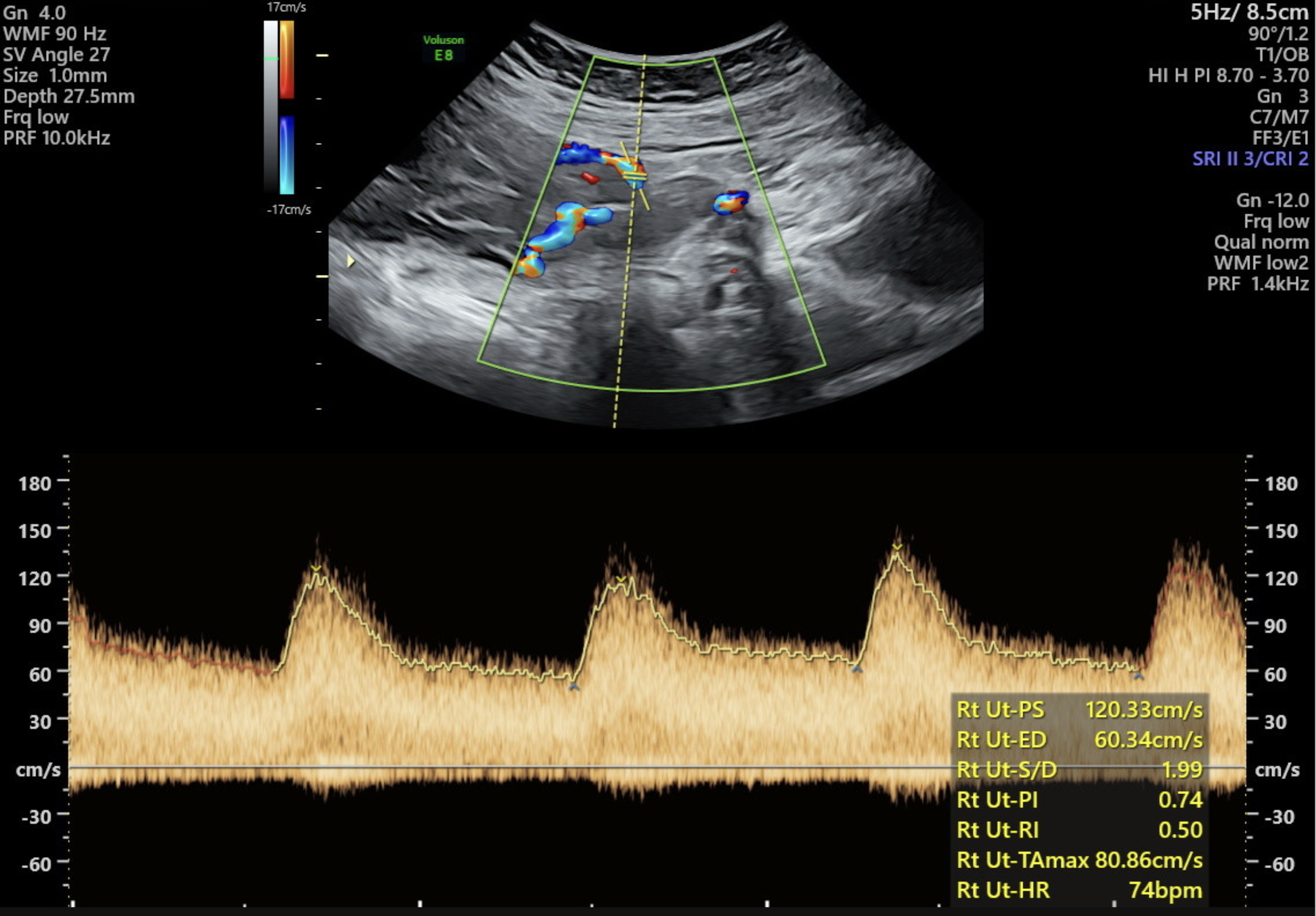
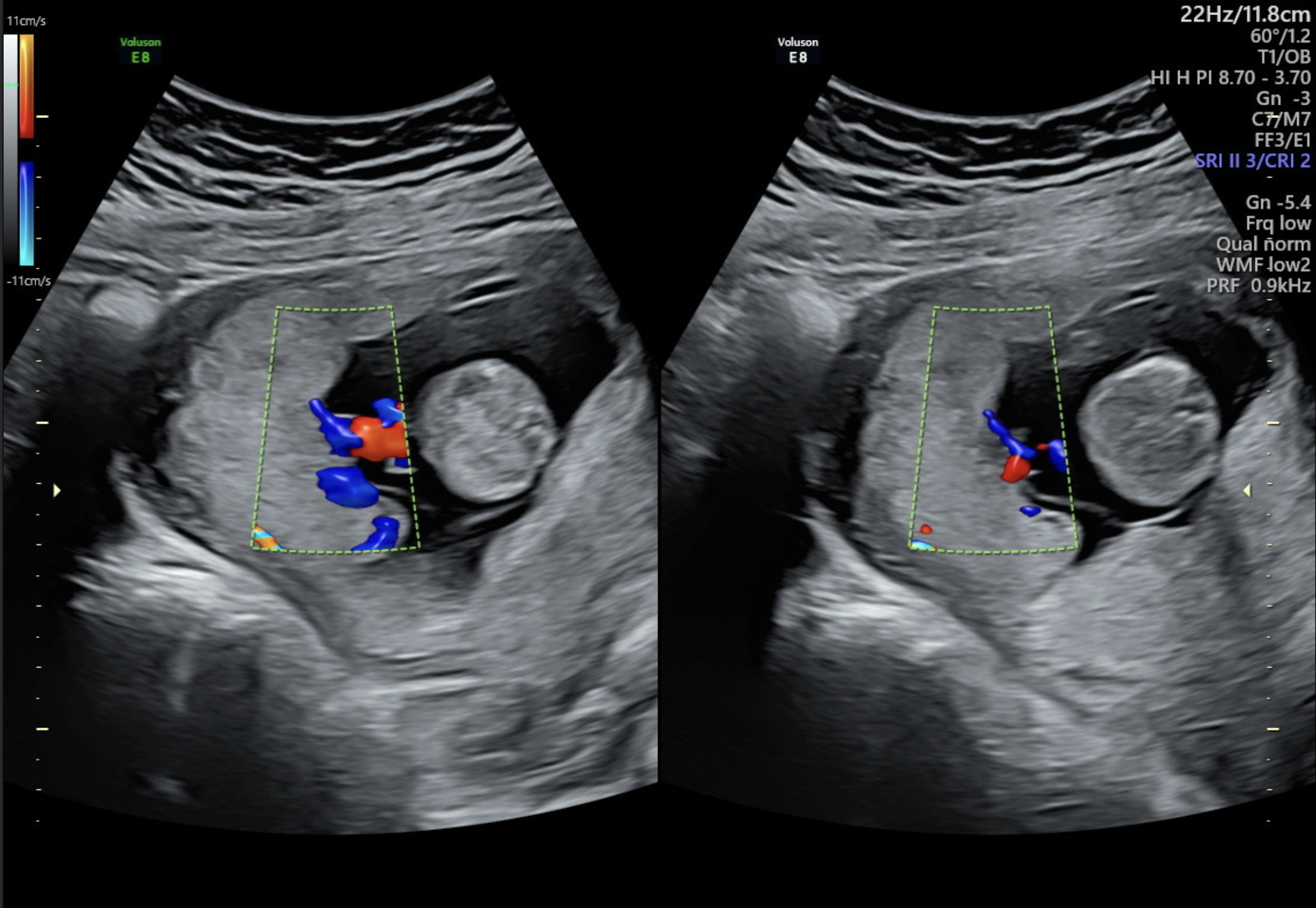
Doppler ultrasound of the right and left uterine arteries
The above parameters and the blood results (PAPP-A and PIGF levels) can identify 75% of women who will develop Preeclampsia and need delivery before 37 weeks. If the results indicate a high-risk developing Preeclampsia, a simple treatment of low dose Aspirin under the direct care of the referring Doctor can help prevent the onset of the most severe type of Preeclampsia.
Before or during your diagnostic ultrasound, our staff will ask you to fill out a basic health questionnaire that will access maternal risks for the development of Preeclampsia.
Your blood pressure in each arm will be taken on the day with an automated blood pressure cuff, as well as your height and weight will be measured on the day.
-
To acquire the best diagnostic images possible, the examination is routinely performed Transabdominally, followed by a Transvaginal ultrasound (always with your written consent first).
Both Transabdominal and Transvaginal scans are safe and are carried out with minimal discomfort. Transvaginal ultrasound is safe to perform during early pregnancy.
The early pregnancy scan typically involves two components: a scan across your lower abdomen with a full bladder (transabdominal scan) and an internal scan (transvaginal scan). The internal scan is a standard practice and does not harm the embryo in any way; it is used to obtain detailed information about early pregnancy. By approximately 8 weeks, the embryo can be readily seen via a transabdominal scan.
-
In most cases the examination will be performed transabdominally, but there are some situations where a Transvaginal ultrasound maybe necessary. This improves the assessment of the cervix, placenta and obtain better details of the fetus. In turn this can improve accuracy if the diagnosis.
Transabdominal and transvaginal ultrasound examinations are safe at all stages of pregnancy.
-
For the best results, we recommend scheduling your appointment as early in your pregnancy as possible to ensure that the procedure can be performed during the optimal timeframe. Use our Pregnancy Scan Calculator to determine the most suitable dates for your scan.
Although a Nuchal Translucency scan or Early Anatomy Screening can be conducted between 12 to 14 weeks, we recommend scheduling this scan at 13 weeks. Our experienced sonographers have found that this specific timeframe allows for optimal visualization of your baby's development, including intricate structures such as the brain, heart, and kidneys. This small window of time can make a significant difference in the clarity and detail of the scan, providing valuable insights into your baby's well-being.
-
For a thorough assessment, it is important to combine ultrasound findings with maternal blood biochemistry. Please ensure to take your maternal serum screening blood test form to any pathology company at least 10 days before your ultrasound appointment. By doing so, we can access these results during your ultrasound. This should be completed from 10 weeks of your pregnancy.
-
The blood test evaluates Beta human chorionic gonadotropin (Free- BhCG) and pregnancy associated plasma protein- A (PAPP-A) levels. While it is ideally conducted at 10 weeks, it can also be performed just before or on the same day as the scan. In cases of fetus’ affected by chromosomal abnormalities, these hormone levels often display abnormalities.
-
While a normal ultrasound can provide reassurance, it's important to note that it does not guarantee a normal baby. Although it can detect most major structural abnormalities, the overall detection rate is only around 60%. Therefore, while ultrasound is a valuable tool, it may not identify all potential issues, and additional screenings and tests may be necessary for a comprehensive assessment of the baby's health.
-
The first trimester screening test involves two main components: a blood test, typically administered at 10 weeks into the pregnancy, and a nuchal translucency scan, usually conducted at 12-13 weeks. Following these tests, the results, along with maternal details, are entered into a computer program developed by the Fetal Medicine Foundation in London. This program then calculates the individual risk for chromosome abnormalities, categorizing it as either "low risk" (less than 1 in 300) or "high risk" (greater than 1 in 300).
-
Description text goes hereThe combined First Trimester Screening is highly sensitive and specific for Down syndrome, detecting around 90% of chromosomal abnormalities. This means that even if the calculated risk is low, there is still a possibility of a chromosomal abnormality such as Down syndrome not being completely ruled out.
-
Receiving a low-risk screening result doesn't guarantee that your baby is free from a chromosomal disorder. It's crucial to understand that this test is only a screening tool and doesn't provide a definitive answer about whether your baby has a chromosomal disorder. In fact, the test can miss about 10% of chromosomally abnormal fetus’.
Furthermore, it's important to note that a low-risk result doesn't guarantee the health of your baby at birth, although the majority of babies are born healthy.
First trimester screening is offered to all pregnant women as a voluntary test, and you have the option to decline if you feel it's not right for you. It's advisable to have a thorough discussion with your partner and doctor before making a decision about whether to proceed with the testing.
-
Although the scan is an important tool for early detection, it may not detect all potential issues. Some structural defects and abnormalities may only become apparent later in pregnancy.
Additional scans and tests may be required later in pregnancy to provide a thorough assessment.
It is advisable to undergo a scan at 20 weeks to assess morphology and placental location. This comprehensive approach helps ensure the well-being of both the mother and the baby.
-
The ultrasound procedure typically lasts around 50 minutes. However, the duration may vary depending on the specific reason for the examination and the complexity of the individual case.
-
If possible we recommend wearing comfortable, loose-fitting clothing that provides easy access to the area being imaged. Two-piece clothing, with separate upper and lower garments, is preferable.
Additionally, please ensure that you empty your bladder 1 hour before the procedure and then drink 2 glasses (600ml) of water, holding it without emptying your bladder again. Please note that your appointment might be delayed if your bladder is not adequately full.
-
Having some urine in your bladder can be beneficial for outlining the cervix and visualizing the relationship of the placenta with the lower uterus during imaging. It also helps to elevate the uterus from the pelvis into the abdomen, facilitating better visualization of the fetus.
You don't need to have a large amount of urine, and simply drinking a glass of water 30-60 minutes before your scheduled appointment is sufficient.
-
We welcome one adult support person, whether it be your partner or a family member, to accompany you during your Diagnostic scan. However, for specific reasons, we have implemented policies that prohibit children from attending Diagnostic ultrasound appointments. While we understand that this may be disappointing for families, it is essential to maintain a focused environment. Thus allowing the Sonographer to be able to concentrate during the scan whilst taking the necessary images and measurements. Occasionally, our sonographer may need to discuss unfortunate news found during your appointment and so this must be taken into consideration. The presence of children can introduce distractions that may impact the quality of the examination.
-
At Trinity Imaging, we provide our patients with their images to an app on your phone. For further details please ask our receptionist at your appointment.

All our scans are performed in our premium-furnished luxury viewing room specially designed for you.
We are all looking forward to getting to know you, your baby and family along your pregnancy journey.